Unless you’ve been living under a rock, you’ve probably heard that there’s a measles epidemic brewing in the United States. As of April 26th, 704 cases of measles have been documented in 22 states across the country. This is the largest number we’ve seen since 2000, when measles was declared no longer endemic in the United States. And the year is not even half over. Cases are destined to rise and, mark my words, we will see death from measles if we don’t get our act together.
(See The New York Times article “Measles Cases Surpass 700 as Outbreak Continues Unabated”)
There are no scarlet letters
Most people in the United States support vaccination. The very large majority of us vaccinate ourselves and our children on schedule. However, small clusters of non-vaccinating individuals are contributing to the return of this highly contagious disease. If these small clusters of individuals kept to themselves, maybe we wouldn’t have such a crisis on our hands. But non-vaccinating folks participate in the larger community just like the rest of us. They go to work and school. They shop at Costco. They attend professional sporting events. They travel the world. There is no identifying mark, no scarlet AV (for anti-vaxxer), that we can use to identify people who are choosing not to vaccinate. And they’re not going around shouting “I don’t vaccinate my kids” from the rooftops. They are, for the most part, hiding in the herd.

Choosing not to vaccinate puts kids at risk
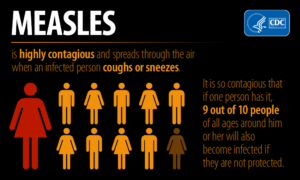
In the name of freedom to avoid the “risks” associated with vaccines – of which there are a documented very few – non-vaccinators are inadvertently raising the risks for themselves and everyone else. The chance of serious or potentially deadly adverse effects from the measles vaccine, or any vaccine for that matter, is approximately 1 in one million. The chance of getting measles if you aren’t vaccinated and are exposed is 9 out of 10. That’s 90%. And of those people infected, 1-2 in 1000 will die. 1 in 1000 will develop inflammation of the brain which can lead to permanent brain damage. 1 in 4 have to be hospitalized.
And don’t forget that people who contract measles develop a sort of immune amnesia. Their bodies seem to forget the immunity that they had previously built to other infections.This puts them at risk for contracting further potentially serious illnesses in the years following a case of measles.
Measles infection also puts a person at risk for developing a universally deadly neurodegenerative disorder, called Subacute Sclerosing Panencephalitis (SSPE), 7-10 years later.
Adults play an important role in spreading disease
And we don’t just have to worry about kids. Kids under 5 are, by far and away, at greatest risk of serious complications if they contract measles. But adults can get measles, too. And adults are much more mobile, which contributes to easy spread of the illness. In the measles outbreak in Michigan, an adult traveling from New York introduced the virus. In the recent exposures in the Seattle area, patient zero was an adult traveling from British Columbia. Adults who are not vaccinated, are under-vaccinated, or who failed to fully mount an immune response to vaccination, can introduce the virus to susceptible populations.
Is it possible we aren’t fully protected?
As adults, here‘s where we stand. People born before 1957 are presumed immune because they likely contracted measles as a child. Though, if you don’t remember having measles or being told by your parents that you had measles, you may want to get your titers checked or just get vaccinated.
The measles vaccine became available in 1963. At that time, there were both killed virus and live virus vaccine options. It was later discovered that the killed virus vaccine rapidly lost its effectiveness, both after initial vaccination and after booster doses were given. Its use was discontinued and, in 1968, both killed and attenuated vaccines were replaced by a much more effective, further weakened live virus vaccine. If you were one of those individuals who received the killed virus vaccine, you may be walking around with incomplete immunity – not fully protected.
In the early years of measles vaccination programs, only one dose was recommended. In 1989, after seeing a rise in measles cases over the years prior, a 2nd dose of vaccine was added to the immunization schedule. One vaccine provides only about 93% immunity and the second dose brings that value up to 97%. However, there will still be 3% of the population who don’t respond to the vaccination. Appropriately, these people are called “non-responders”. These folks, and those who cannot be vaccinated because of immune suppression, pregnancy, or being too young to get the vaccine, rely on the rest of us – their community – to maintain a bubble of immunity around them.

Creating an immunity community
There are certain groups who are often required to prove immunity to vaccine preventable diseases. This is typically done by documenting 2 MMR vaccines or the measles illness. Immunity can also be demonstrated through the testing of titers. These include people in the medical field, those in public education, and public health professionals who are “first responders” in the case of an outbreak. All of these folks, who care for you and for your children, must be able to demonstrate immunity. But what about the rest of us? What role do we play in protecting our community? What can we do to help limit the spread of disease?
I’m so glad you asked! In an outbreak situation, all of us have a role to play in protecting ourselves and those around us. Here are a few things you can do to help.
- Get vaccinated. If you are someone who was initially hesitant about the vaccine, but now worry that you or your child may be at risk, vaccinate! Talk to your doctor or public health department about how to catch up on your immunizations.
- Get tested. If you were born between 1963 and 1989, consider testing your titers to see if you are immune. If not, get an MMR booster!
- Know before you go. Travelers are at high risk of contracting measles. It is not necessarily people coming from other countries that bring disease to us. Most often it is unvaccinated Americans who travel abroad and return home, bringing vaccine preventable diseases with them. Before you travel, check to see what’s circulating in the country or countries you will be visiting. And make sure that you are up to date on your immunizations.
- Ask the question. Though it may be a bit uncomfortable to ask, you need to know if the people that you and your children spend time with are vaccinated. This is particularly true if you fall into one of the high risk categories (pregnant women, people with suppressed immune systems, infants under one year of age, etc.).

Talk about spreading false info! Wow! 0.0000023466% of cases in the US. Again cases… there have been ZERO deaths!
But hey 609,000 people DIED of cancer last year (12,000, of them children), yet you aren’t too concerned about all the carcinogens in our food supply, environment, and yes vaccines.
Over 500 people DIED in plane crashes last year.
So let’s get a grip. Measles is a mild childhood illness. Maybe you need to go back to me school and get some refreshers?
Oh, frustration. Lost my initial comments. Ok, I’ll try again. In a nutshell…there have been zero deaths and decreased incidence of measles BECAUSE of vaccines. If you don’t get the illness, you can’t die of it, right? And I totally care about all sources of morbidity and mortality and am very focused on prevention. As a family physician, prevention is my passion. I find it interesting that people suggest that if I am focused on vaccination that I somehow am ignoring all the other important interventions for health. It is not either/or it is both/and. There are many forms that prevention takes but vaccination is by far and away the most effective public health preventive measure we have. Speaking of cancer, I HIGHLY recommend preventing cervical, vulvar, vaginal, rectal, anal, penile, and oropharyngeal cancers by giving the HPV vaccine. Who doesn’t want to prevent cancer? And 80,000 people died in the US of the flu last year, >80% of whom had not had their flu shot. Flu shots save lives. Thanks for your concern about my education but I am well versed in the topic of vaccines and vaccine preventable disease.