We’ve been successfully vaccinating children against Hepatitis B since the early 1990s. And, in the past, only “at risk” adults (those with exposure to blood and body fluids through work or lifestyle) were recommended to receive the Hep B vaccine series. But this summer, the CDC’s Advisory Committee on Immunization Practices (ACIP) updated guidelines to recommend Hep B vaccination for the large majority of adults. In today’s blogpost, we’ll discuss the dangers of Hepatitis B infection, why the recommendations are changing, and who qualifies for Hepatitis B vaccination. Hang on as we discuss Hepatitis B vaccines for adults – preventing a deadly disease.
What is Hepatitis B?
Hepatitis B is a contagious virus that infects the liver. Its siblings, Hepatitis A and C, can similarly cause liver damage. While hepatitis A spreads via contaminated food and water, hepatitis B and C spread through contact with infected blood or body fluids. There is no vaccine for Hepatitis C at this time but we do have a highly effective vaccine against Hepatitis B. And thankfully so.
While many people do not experience any symptoms of a new “acute” hepatitis B infection, some may develop liver inflammation with associated yellowing of the eyes and skin (called jaundice), nausea, vomiting, abdominal pain, dark urine and extreme fatigue. Most people’s body’s will be able to fight off this infection, resulting in lifelong immunity. However, some will then go on to develop chronic Hepatitis B infection which, decades later, can result in liver failure, liver cancer, and death. This is what we are trying to prevent.
Why do we vaccinate infants?
The hepatitis B vaccine became available in the 1980s but didn’t become part of the routinely recommended vaccinations for children until the 1990s. Prior to this, we were attempting to use this vaccine primarily for those who were “at risk”. However, using this approach didn’t make much of an impact on rates of Hep B transmission. Why? Because you can’t just look at someone and tell who is “at risk”. It wasn’t until we started vaccinating babies that we began to see decreasing rates of Hep B.
We vaccinate to decrease transmission but also to decrease significant harm from illness for the person receiving the vaccine. In the case of Hep B vaccination of infants, we also vaccinate because babies who come into contact with Hepatitis B are much less able than adults to fight off the virus. Up to 90% of babies exposed to Hepatitis B will become chronically infected and this chronic infection means a shortened lifespan for them and possible transmission to others.
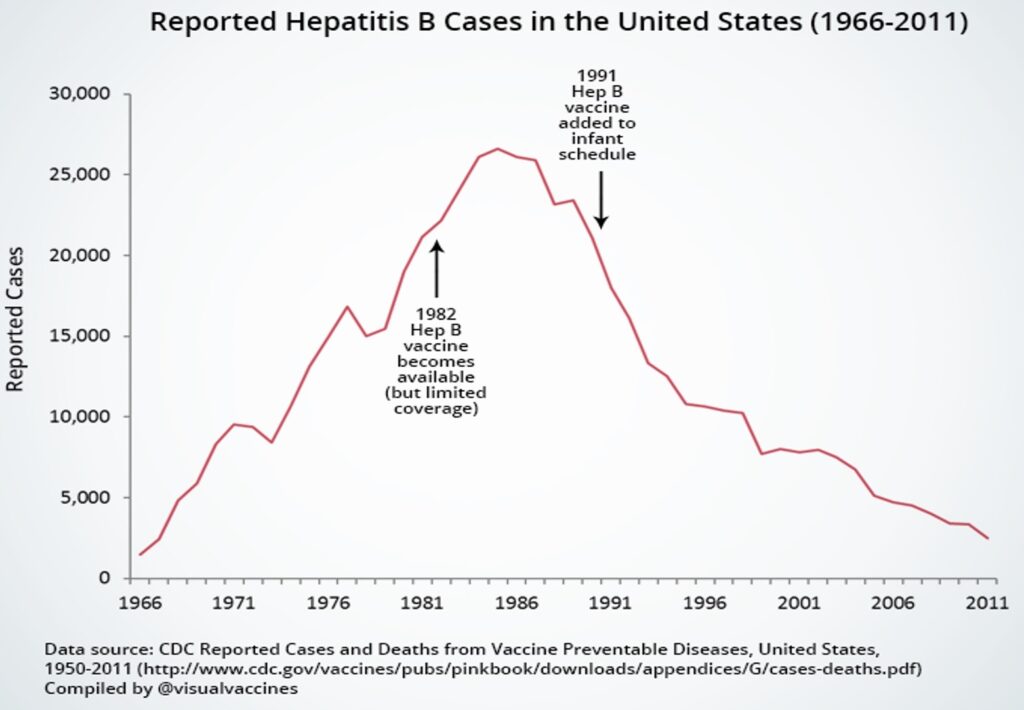
Graph showing no improvement in US rates of hepatitis B infections when an “at risk” approach was used. Not until the vaccine was added to the infant immunization schedule did we start to see a drop in community rates.
Some parents may ask, “Why can’t we just test the mother and only immunize those babies whose mothers are positive for the virus?”. The answer is that, in up to two-thirds of cases of neonatal hepatitis B infection, the mother tests negative and the baby is infected by a family member or caregiver.
How common is Hep B?
The CDC states that approximately 1.2 million people in the US and 350 million people worldwide are infected with hepatitis B. 50-70% of those infected don’t have any symptoms and don’t know they have it. More than 3000 in the US and 600,000 worldwide die annually from Hep B-related liver disease.
Who should be vaccinated against Hep B?
There are some obvious groups; people like doctors, nurses, dentists and others who work with blood and body fluids in the medical field, or those with injection drug use or multiple sexual partners. But it doesn’t take intimate or risky behavior to contract hepatitis B. For example, people who live or work in homes for the developmentally disabled or correctional facilities are also at increased risk. Here are the CDC’s guidelines for Hepatitis B vaccination. See if you fit into any of these categories…
- ALL people ages 0-59 years old
- Anyone who wants a hepatitis B vaccine
- Anyone who is 60+ years old and has a high risk indication for vaccination:
-
- People with Diabetes
- People with HIV infection
- People with end-stage renal disease, including those on dialysis
- People with chronic liver disease, including Hep C, cirrhosis, fatty liver disease, autoimmune hepatitis, ALT or AST levels greater than twice the normal level
- Travelers to regions with increased rates of Hep B
- People living or working in correctional facilities
- Residents and staff of facilities for developmentally disabled persons
- Health care and public safety workers at risk for exposure to blood or body fluids
- People living with someone infected with the Hep B virus
- People who share needles, syringes, or other drug-injection equipment
- Men who have sex with men
- Victims of sexual assault or abuse
- People seeking evaluation or treatment for sexually transmitted disease
- Sexually active people who are not in a long-term monogamous relationship
- People whose sex partners have Hep B
But why do I need the vaccine if I don’t have any risk factors?
As discussed above, the majority of people walking around with hepatitis B have no symptoms. And they don’t know they have it. This means they wouldn’t necessarily be taking any precautions to prevent transmission. What’s equally worrisome is that, of those that have hepatitis B infection, 30-40% have absolutely NO risk factors (how could this happen? see discussion below). This is why the decision was made to vaccinate more broadly than just during infancy.
Let’s look at some low-risk scenarios for kids and adults where one could become infected:
- A baby with a chronic hepatitis B infection bites another child or their daycare provider at daycare
- You are volunteering at the local homeless camp and you get saliva or tears from an infected person into an open cut. Hepatitis B can last on surfaces for up to 7 days! Yikes!
- You are playing a contact sport, where skin and mucosal injuries are common, and there is blood transfer from an infected person’s wound into your own
- Someone could use the razor or toothbrush (gross!) of a friend or family member who doesn’t know they have hepatitis B
- A relative or daycare provider chewing food for a baby could transmit hepatitis B from the infected adult to the infant
Why is Diabetes a risk factor?

Image showing finger stick blood sugar testing. Exposure to blood can increase the risk of infection with hepatitis B. Image from Pixabay.
People with Diabetes are most often checking their blood sugars using finger sticks. It is not uncommon that spouses or children will use their diabetic family member’s lancets to check their own blood sugar. This can transmit the illness. People with diabetes also tend to have medical issues that may land them in a medical or rehab facility where others are in charge of blood sugar monitoring. The potential for inadvertent blood transfer is greater in medical facilities. Also, diabetes adversely affects the body’s ability to heal. If someone with diabetes gets exposed to hepatitis B, they are less likely to be able to fight it off and it can more easily become a chronic infection.
Tell me more about the vaccine itself.
- What type of vaccine is it – The hepatitis B vaccine is a recombinant protein, killed virus vaccine. This means there is NO active virus present so it CANNOT cause hepatitis B.
- How many shots do I need – Traditionally, it is a three shot series given over a period of 6 months. In children, it is typically given within 24 hours of birth, and then again at the 2 and 6 month well child checks. There is also a two-shot option available for those 18 and older, administered 4 weeks apart.
- Will I need boosters – We typically consider this a “one and done” set of shots (at least for now – as we know, science is always learning and adapting and recommendations can change). It induces long-term immune memory, up to 30 years, and protection continues even after antibody levels fade.
- How effective is it – 90-95% of people will mount a lasting immune response to the vaccine. Those who don’t are considered “non-responders”. Non-responders may receive the vaccine series once more but we stop immunizing if they still don’t respond. Those folks would need Hepatitis B immune globulin with a known exposure to hepatitis B. Of those who respond, the vaccine is 80-100% effective in preventing infection for those who receive the full three dose series.
- Are there any side effects – The most commonly reported side effect of the hepatitis B vaccine is a sore arm. However, allergic reactions can happen. It is for this reason that we recommend that people with yeast allergy avoid the Hep B vaccine since the recombinant proteins used to develop the vaccine are grown in yeast cells.
- Is the vaccine safe – Studies show NO association between the vaccine and any increase in fever, sepsis, new onset allergies or brain problems. They also find NO association between Hep B vaccination at birth and neonatal death.
What if I don’t know if I’ve already had the shots or if I’ve already been infected?
Simple blood tests can be done to detect exposure to or immunity to hepatitis B. Image from Pixabay.
We can easily sort this out by doing some simple lab work. Your clinician can order a series of tests that look at antibody and antigen (viral protein) status. These can help define if you are immune. They can also help you determine if there was a prior infection and if you have successfully fought off the virus or remain infected and contagious. It is not uncommon that people think they’ve been vaccinated before but aren’t sure and don’t have any records. In that case, we check antibody titers. If elevated, they prove immunity. No further vaccination is necessary.
Are there any groups who should be screened for infection?
The answer is, yes! The following groups should receive screening for hepatitis B infection:
- People born in countries with a prevalence of Hep B infection >/= 2%
- People born in the US not vaccinated as infants and whose parents were born in regions with high rates of Hep B infection
- Men who have sex with men
- People who inject drugs
- People with HIV
- Household and sexual contacts of people with Hep B infection
- People requiring immunosuppressive therapy
- People with end-stage renal disease (including those receiving hemodialysis)
- Blood and tissue donors
- People with elevated alanine aminotransferase levels
- Pregnant people
- Infants born to people with Hep B infection
Well, there you have it – everything you ever wanted to know about Hepatitis B immunization. If you were a child in the decades preceding the 1990s, you are my people. But also, chances are you need this vaccine. If you have diabetes (that’s nearly 11% of the US population), chances are you need this vaccine. If you are not in a monogamous relationship, chances are you need this vaccine. Etc, etc, etc. When you are out there getting your flu shot and your bivalent COVID booster (wink, wink, nudge, nudge), talk to you clinician or pharmacist about catching up on the hepatitis B series of vaccines.
Thanks for reading! If you would like to receive updated vaccine information directly to your inbox, please hop on over to the homepage and subscribe. And please share this article with friends and family. Many of our vaccine recommendations can fly under people’s radar. We in the medical community appreciate all the help we can get in spreading the word! Until next time…

