To mask or not to mask – that is the question… among many many others. It’s now been over a month since I started writing about the novel Coronavirus that hit our world like a ton of bricks. In that time, what we know, or think we know, about this virus has changed. Likewise, guidelines and recommendations for managing and controlling the virus have also changed, like those for wearing masks. And all this change can be confusing. We’ll come back to this later.
The general public is getting a glimpse into aspects of medical care that few, other than medical personnel, ever see. The chinks in the armor of our healthcare system, as well as those in our national emergency preparedness plans, are on full display. Our systematic undervaluing of science and public health is coming back to bite us you know where.
There will certainly be many lessons to learn from this experience. As a nation, if we are to make the most of this education, we must start from a place of humility. We need to admit our failings so that we can improve and keep from repeating our mistakes. And we don’t have to wait until the pandemic is over to begin taking note of better ways to get things done. This education starts now.
Image adapted from Pixabay
Today, we will explore some of the lessons we’ve learned. We will review some of the medical terminology and therapeutic approaches to help the non-medical public make sense of what they are hearing on the news. We will look at how some countries are managing this pandemic better than we are. And we’ll review what’s on the horizon. Thanks for joining me again and I look forward to hearing your thoughts and feedback!
First, let’s talk terminology
During this pandemic crisis, lots of medical and scientific terms are being thrown around and they don’t always make sense to the general public. Let’s look at some of these and maybe this will help people better understand what’s happening in those ICUs and why we are doing what we are doing.
• ARDS (Acute Respiratory Distress Syndrome) – As a result of injury to the lungs, as can happen in the setting of COVID19 and other serious infections (like the flu), fluid fills the tiny airspaces of the lungs and prevents oxygen from passing into the blood stream. This causes a process similar to drowning. Supplemental oxygen and ventilators are used to increase oxygen delivery and to push fluid out of the airspaces. Without ventilators, people suffering from ARDS often die.
• Proning – If you’ve been watching the news, you’ve undoubtedly seen images of patients in the ICU, face down in their beds. This looks odd but patients are placed in this position for a very important reason. This is called the prone position and it helps people with ARDS to make the most of their healthy lung tissue. Let’s look at a graphic from the Canadian Respiratory Journal that helps explain why this works.

Note: the triangle in the image represents the spine and the oval represents the heart. The supine position is when the patient is lying on their back and the prone position is when the patient is lying on their front. The dark shading indicates areas of the lung that have poor oxygenation. The lighter shading indicates good oxygenation. You can see that with the patient lying supine (on their back), the heart takes up needed space in the well oxygenated part of the lung. While lying prone (on their front), the heart takes up space in the poorly oxygenated part of the lung, leaving more space for well oxygenated lung tissue. In ARDS, the more oxygenated lung tissue the better!
• Convalescent plasma – to “convalesce” means to “recover from”. As the body is recovering from a viral infection, it develops antibodies (the weapons of the immune system) against that infection. Antibodies are what keep us from getting sick with that same illness again in the future. Using convalescent plasma as a treatment means harvesting antibodies from the blood of someone who has recovered from COVID-19, and giving those antibodies to someone who is currently struggling with the infection. Giving that ill person a dose of antibodies against the infection can help them fight it off and increase their chance of survival.
This method of treatment is being tested in various locations around the world and is showing some promise. However, it is a cumbersome process and difficult to ramp up to large scale. And it is not yet clear if it will be helpful in those that are critically ill or would need to be given earlier on in the disease process.
• Antibody testing – the current SARS-CoV-2 test looks for the virus’ genetic material to identify an active infection. But what will be equally, if not more, valuable to know is when someone becomes immune to the virus (when they have developed antibodies). There are different types of antibodies. Those that are produced early to fight active infection are called IgM antibodies. Those antibodies that are produced later, as recovery begins, and stick around to fight off future infections with the virus are called IgG antibodies.
Testing can differentiate these two types. A predominance of IgG antibodies means that someone has recovered and is now immune. The level of IgG antibodies can then be monitored over time and will tell us how long immunity lasts. For people who have no symptoms or minimal symptoms, it can tell us who has been exposed and will allow easier contact tracing and isolation of those contacts. Antibody testing is just being approved and will likely be available for more general use by the end of April.
Next, let’s discuss concepts in medication and vaccine development
This novel Coronavirus is a virus, right? Why can’t we just use antiviral medications to treat it? And what about Hydroxychloroquine? Some think this can be helpful. Can’t we just get this to everyone that is diagnosed with SARS-CoV-2? We already know how to make vaccines. Why can’t we just plug in the information about the Coronavirus and come up with a vaccine right away? These are really good questions and ones I hope to give you an answer to. The first thing we need to understand is that the process of developing medications and vaccines is long and involved. It doesn’t happen overnight.
With medications, we are treating people that are ill. But with vaccines, we are giving a medical intervention to a completely healthy person. We have a very high threshold for safety when we are giving something to people who are totally well. Not that we care less for safety when treating people who are sick, but treatments during sickness are more urgent. Patients are more willing to accept some small amount of risk and uncertainty when they are ill than when they are healthy.
It generally takes years to develop new medicines. However, studies looking at new uses for existing medications are easier to conduct. And in a pandemic scenario, these studies happen much more rapidly than normal because we are desperate to find anything that will help. As a result, you may see the FDA fast-tracking use of therapies that they would otherwise spend more time investigating. But desperate times call for desperate measures.
However, we still have to prove that we are not doing more harm than good when we use a medication in an out-of-the-box way. This is why scientists are so hesitant to give a free-for-all go-ahead to use of Hydroxychloroquine and Chloroquine to treat COVID-19. Even though there is suggestion of promise, these medications need to be studied against placebo or other treatments to prove their effectiveness and safety. Additionally, they are currently in short supply so liberal use of these medications is not in our immediate future.
Regarding antiviral medications, they are not a one size fits all treatment. Antiviral medications are specific to certain viruses. The antiviral for influenza does not treat herpes, for example. And the antiviral for herpes does not treat HIV, and so on. At their core, viruses have some similarities and it is possible that an antiviral for a particular virus could benefit someone with a different virus. We try our existing antivirals in patients with COVID-19 because we are searching for anything that might help.
In the case of vaccines, the development process typically takes much longer than that of medications, sometimes decades. There are now numerous trials around the world hunting for an effective immunization. And, really, the more the merrier since most vaccine trials eventually fail.
While usually slow, production of a SARS-CoV-2 vaccine is proceeding more rapidly than normal. This is because work to develop a vaccine against other coronaviruses had already begun. Scientists have been working on vaccines for SARS and MERS, which share genetic similarities with the SARS-CoV-2 virus, since these viruses caused their own outbreaks. The legwork is already done. But we are many months (likely 18-24) away from a successful vaccine as these candidates now have to be tested on humans.
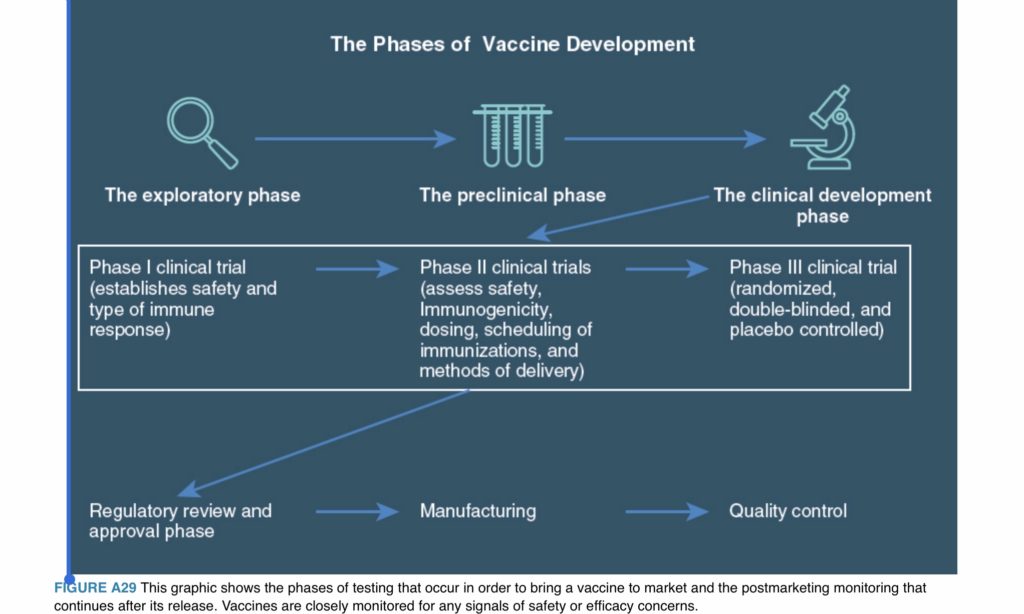
Taken from Let’s Talk Vaccines: A Clinician’s Guide to Addressing Vaccine Hesitancy and Saving Lives, Wolters Kluwer Press 2019, Gretchen LaSalle, MD
Human testing goes through several very important stages, starting with a low number of participants. These initial studies look at tolerability, safety, and the ability to induce an adequate immune response. If successful, they proceed further up the testing ladder, using greater and greater numbers of test subjects.
Subsequent testing phases continue to monitor for safety and effectiveness. They watch for adverse reactions that might be noted only when the immunization is given to larger numbers of people. This process is necessarily slow and methodical. We want our interventions to work and to be as safe as possible. Slow and steady wins the race.
Let’s explore changing guidelines
I promised I would get back to the seemingly ever-changing mask guidelines, so let’s get to it now. First the CDC says that your average non-ill, non-medical person should not wear a mask. Now, it seems they want everyone to wear masks. What’s changed? And if healthcare workers are only allowed to wear surgical masks or N95 masks, why are cloth masks ok for the general public?
First, we must recognize that the initial guidelines were not based on what was medically best. They were based on what was necessary. In an ideal situation, we would have had enough masks for medical professionals and the public alike. But we did not. A lack of supplies drove our initial guidelines and medical masks had to be conserved for medical providers.
Initially, it was also felt that the virus spread primarily by respiratory droplets from those that were ill. Adequate physical distancing was felt to limit spread and controlling the coughs and sneezes of those with symptoms was of utmost importance. Thus, masks for symptomatic patients were also recommended.
However, with further study of this new pathogen, we now suspect that viral particles may also aerosolize (float in the air for extended periods). It is thought that they can even spread from infected but asymptomatic people, through merely talking or breathing. Armed with this knowledge, masks for everyone now seems most prudent.
If we had enough surgical masks for all, then these would be advised for common use. But we are still struggling with a lack of personal protective equipment for our medical and hospital staff. This is why homemade cloth masks are deemed acceptable. They are certainly better than no mask at all. Click here to see a quick and easy way to make your own cloth face mask.
Please note – this does NOT mean that we can stop our 6 feet social distancing. This is merely meant to augment those efforts when settings require closer contact (like picking up prescriptions from the pharmacy, for example, or walking past people in the grocery store).
Public Service Announcement:
If you are wanting to avoid any criticism of our federal leadership’s response to this pandemic, you should stop reading now.
In my humble opinion, the president needs to follow CDC guidelines just like the rest of us. People look to him to know how seriously to take this pandemic and he has done a brilliant job of minimizing and undercutting the recommendations of scientists and public health officials. He needs to lead by example and do what is best for his people, not merely what is convenient or easy.
What have we learned from other countries?
There is no doubt that other countries were better prepared for this pandemic than we were. Funding cuts to the Centers for Disease Control and Prevention and dismantling of the pandemic response team in the years prior to the pandemic put us at a significant disadvantage in dealing with this emerging threat in a quick and nimble way. And our federal response has been, at best, wishy washy.
There is little in the way of a nationally coordinated approach, informed by science and public health best practices. The states have been left to their own devices to set expectations and guidelines for their citizens, some acting more decisively than others. Additionally, the states’ governors are told to fend for themselves in acquiring the necessary equipment to keep their medical professionals and public safe. This pits them against each other in bidding wars for supplies, which is beneficial to no one.
Other countries, like South Korea and Germany, have been more successful in flattening the curve. Some of what we are seeing there is a numbers game, true. They began testing earlier and in greater numbers than we did. The greater the number tested, the greater the number of people who test positive. These people are then counted in the total number of citizens affected. A larger COVID-19 positive denominator means a seemingly smaller percentage of people dying from this disease. The math makes a difference and it may be making their death rates look, relatively, better. If we had enough tests, we would do the same.
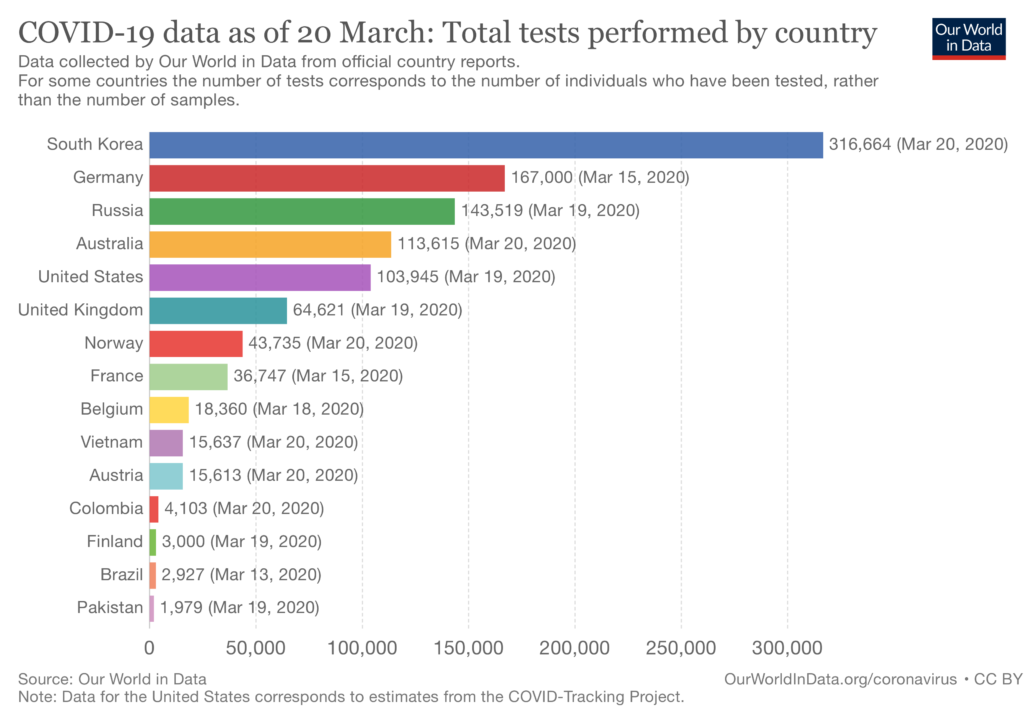
Testing numbers from Our World In Data
But knowing who is infected, whether or not they have symptoms or progress to needing intensive care, also allows those countries to more aggressively and more quickly isolate people. This slows the spread. And infected persons can be monitored more closely, with high risk people or those with early signs of worsening being transferred to higher acuity care, sooner rather than later. Early intervention (if that intervention is available) increases the chance of survival.
What’s the take away? We were slow to recognize the seriousness of this threat and we underestimated the virus’ potential for devastation.
What’s on the horizon?
1. More masks?
Well, not really. But sterilization machines are being deployed to various spots around the country which will allow tens of thousands of masks to be decontaminated each day. They will then be safe for re-use, minimizing the total number of masks needed to keep front line healthcare workers protected.
2. Apps to track the virus?
Technology is amazing. And with the world in 24/7 constant contact through the Internet and social media, why not make use of this fact to track the virus in real time? This is exactly what countries like Britain and Israel are doing and the US may be next to adopt this approach. Internet and App surveys are used to ask questions about symptoms (sore throat, cough, shortness of breath, loss of sense of taste and smell) and to gather temperature data. This may allow us to track the illness and isolate people more aggressively.
3. A doctor draft?
Not exactly like the NBA. More like World War II. This is being proposed by Mayor Bill de Blasio of New York, one of the hardest hit cities in the US. Will we be called to move from one part of the country to another to aid the war effort? Or does this mean that those in retirement will be called back to service? It is not yet clear. These and other ideas to increase our medical workforce are under consideration.
4. Testing for immunity?
As discussed earlier, tests for antibodies to the SARS-CoV-2 virus have recently been approved by the FDA and should be ready for prime time in the coming month. This may be a game changer for how we track this disease and how we make decisions about who can get back to work and when.
In memoriam
I’d like to take this opportunity to remember all of those who have fallen to this devastating disease. Specifically, I’d like to honor the medical professionals who ran into the fire and the fight and were taken from us too soon. Medscape has compiled a list and will be updating it periodically. You can click here to see the names of these fallen heroes from around the world.

Image from Pixabay
A prayer is appreciated but you can better honor them by staying home. Don’t become the next victim that we have to take care of.
Be safe and take care of each other!
Gretchen LaSalle, MD FAAFP


Thank you for continuing to help keep us informed.
Thank you for this blog and it’s amazing contribution to our community (and world)!
Thank you for taking the time to clarify many questions people have.
I hope we hear from you again.
Pray for the people of the world
Thanks Gretchen-the information you are providing is helpful!
Thank you so much for this most informative article!
It’s my pleasure, Maggie!
Be well!
Another well written and informative article, Dr. LaSalle. Thank you for being a voice of wisdom in such uncertain times.
Thank you, Kari!
Thanks Gretchen! Your blogs are fantastic….easy to read, informative and to the point, and with all the appropriate detail. I think everyone should read these, because you cover all the issues in an easy to understand writing style. Stay safe!
Thank you, Linda! I hope you’re doing well and you and your family are staying safe!
Thanks Dr. LaSalle, you are a great doctor. I would like to see more guidance for the public on what to do exactly for the different stages of COVID. From the media reports, it sounds like you go from healthy to being on a ventilator which is, of course, terrifying. There must be treatments for symptoms that we can prepare to have at home. I’m afraid people panic and go to the hospital or call 911 too soon, which uses emergency personnel and PPE unnecessarily. We need more practical help without hysteria. Thanks.
Hi Doris! Good to hear from you. It’s tough since we don’t really yet know what helps. There are certainly supportive therapies (guaifenesin expectorant, inhalers for people with asthma or COPD, fluids, Tylenol, rest, etc.). But it’s true, this virus can take a sudden turn for the worse and we have to take any significantly worsening symptoms seriously. We will know more about the virus and treatment in the next few months, as more and more studies are carried out looking at various treatment options at different stages of illness. Be safe!
Thank you so much, Gretchen. I appreciate the way you approach and provide this information.
Thanks, Carrie!
Dr. LaSalle, I see many pods of people in parks ect. My family meets friends/family in the park for short visits, and we remain AT LEAST 6 feet apart. It has been great for my mental health to say hello and have some social time in the fresh air. If we our OUTSIDE and stay at the minimum distance, IS THIS SAFE ?
Hi BethAnn,
That’s a really good question. I completely understand the need to see family and friends but everyone really has to be willing to abide by the letter of the law. No exceptions. I think if there are no children or animals in the equation (as I wouldn’t trust them to keep at least 6 feet apart) and there is no communal food or drink and people truly are more than 6 feet apart in all directions, it is probably ok. To make it even safer, you could consider wearing your masks.
Well written and very informative. Thank you for your earnest contribution to keeping us informed!
Thanks, Tamara!